The rise of telehealth has reshaped healthcare delivery, moving from a niche service to a fundamental component of patient care for many practices. While the initial scramble to adopt virtual visits might be over, the challenge now lies in making telehealth seamless. Cumbersome workflows, disconnected systems, and administrative hurdles can negate the efficiency benefits telehealth promises. Proper integration means weaving virtual care into the fabric of your daily operations, making it as natural and efficient as an in-person visit. Achieving this requires leveraging the right tools, particularly your Electronic Health Record (EHR), and understanding the specific documentation demands of virtual encounters.
Overcoming Challenges of Standalone Telehealth Platforms
Many practices initially adopted standalone telehealth platforms out of necessity during the COVID-19 pandemic. While functional, these often create information silos and require duplicate data entry, disrupting established routines. Staff might find themselves juggling multiple logins, transferring patient information manually, or struggling to reconcile virtual visit notes with the main patient chart. This digital friction adds complexity and increases the risk of errors, undermining the goal of making healthcare delivery more straightforward and efficient. The key to overcoming this is to centralize telehealth functions within the system your practice already relies on: the EHR.
Leveraging Your EHR for Seamless Telehealth Integration
An EHR like PymedOne, designed with telehealth in mind, serves as the command center for both virtual and in-person care. Specific features are crucial for smooth telehealth integration when evaluating your current EHR or considering a new one.
Integrated Scheduling and Reminders
Integrated scheduling is paramount. Your system should allow staff to book telehealth appointments directly within the main schedule, using distinct appointment types or color-coding for clarity. Automated appointment reminders sent through the EHR's patient communication tools should specify whether the visit is virtual and provide necessary connection details.

Secure Built-in Video Conferencing
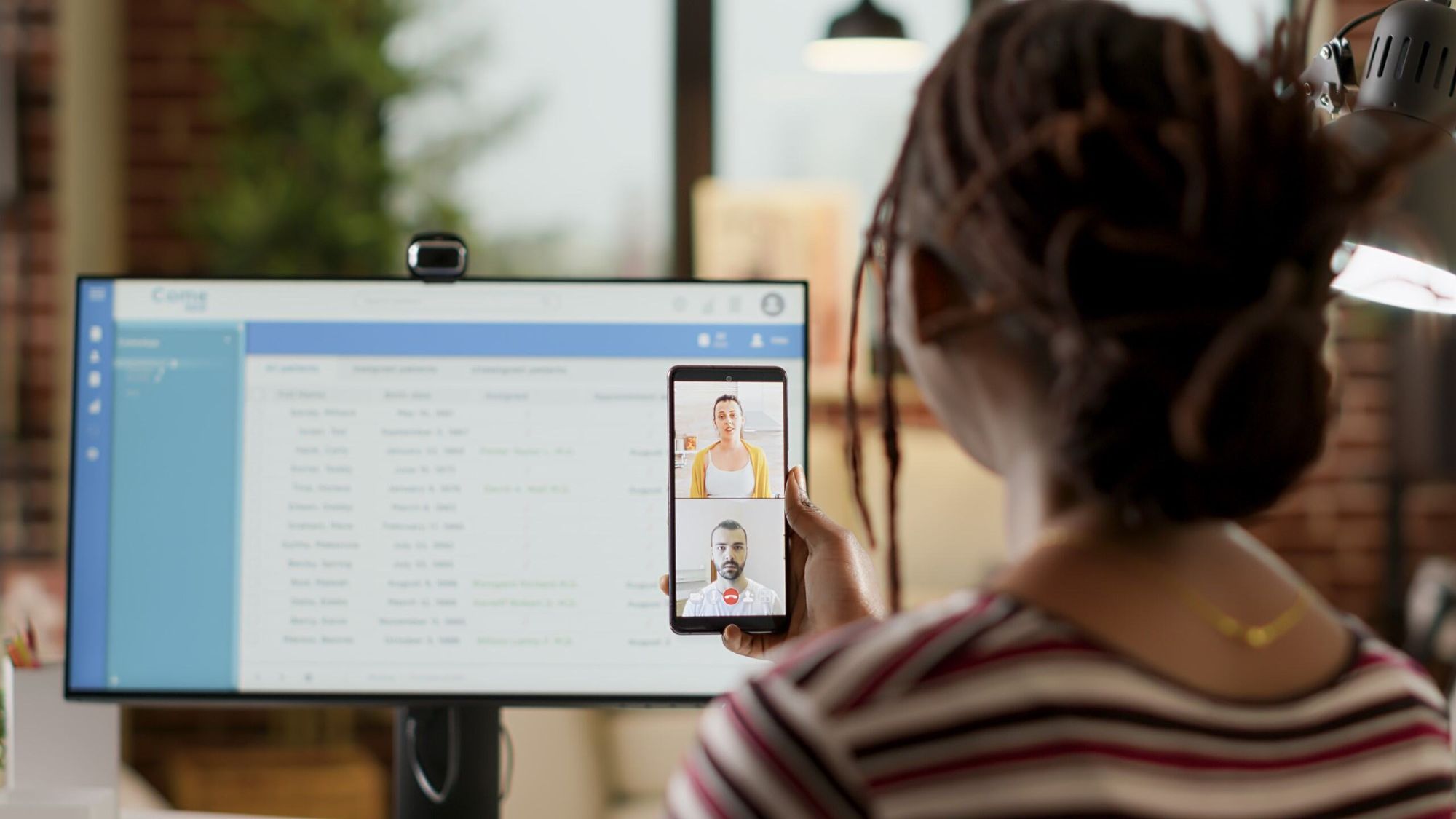
Look for EHRs with secure, built-in video conferencing platforms or deep integrations with HIPAA-compliant third-party services. Launching a virtual visit directly from the patient's chart or the daily schedule saves valuable time and eliminates the need for separate applications. This close integration ensures that the connection is secure and that the context of the patient encounter is readily available to the provider.
Streamlined Patient Portal Access
Patient portal integration further streamlines the process. With an ideal EHR setup, patients should be able to access their scheduled telehealth appointments, complete pre-visit questionnaires or intake forms electronically, and launch their virtual visit directly from the portal. Secure messaging via the portal can also facilitate pre-visit communication or post-visit follow-up, keeping all interactions tied to the patient's record.
Efficient Documentation, e-Prescribing, and Billing Support
Clinical documentation tools within the EHR must also support virtual care. Configurable templates tailored for telehealth encounters can prompt providers to capture relevant details specific to a virtual setting. The ability to efficiently document history, observations (adapted for a virtual medium), assessment, and plan during or immediately after the video call, directly within the patient's chart, is essential for maintaining continuity and saving time. Seamless e-prescribing and order entry functionalities mean that any necessary medications or follow-up tests identified during the telehealth visit can be ordered immediately within the same system workflow. It is also essential to have strong support for billing and coding. Your EHR should facilitate the easy selection and application of appropriate telehealth billing codes, modifiers, and place-of-service codes, reducing claim errors and ensuring proper reimbursement.
The Critical Role of Telehealth Documentation
Beyond the technology itself, meticulous documentation remains a cornerstone of compliant and effective telehealth. While the core principles of good clinical documentation apply, virtual visits have unique requirements. Always begin by obtaining and documenting the patient's informed consent to receive care via telehealth. This confirms that the patient understands the nature, risks, and benefits of a virtual visit.
Essential Documentation Details for Compliance
Precisely document the start and end times of the telehealth session, as this is often crucial for billing purposes. It's also vital to record the physical location of both the patient and the provider during the encounter. State licensing laws and payer regulations often depend on these locations. Note the specific technology platform used for the visit (e.g., your EHR's integrated video feature or a third-party app).
Documenting the Virtual Clinical Encounter
The clinical note itself should mirror the thoroughness of an in-person visit note, including chief complaint, history of present illness, relevant review of systems, and pertinent physical exam findings (describing how these were assessed remotely). Document your medical decision-making, assessment, and care plan. It is important to note any limitations encountered due to the virtual nature of the visit. This includes the inability to perform certain physical examination maneuvers, or any technical difficulties experienced by either party. This transparency safeguards both the patient and the provider.

Practical Steps for Successful Implementation
Integrating telehealth seamlessly is not just about adopting technology; it involves refining workflows and ensuring compliance. Map out your current telehealth process, identify bottlenecks, and see where EHR features can smooth the path. Invest time in training clinical and administrative staff on using the technology, the integrated workflow, and specific documentation protocols. Educate your patients as well, providing clear instructions on how to connect to visits and use patient portals effectively.
Achieving Efficient and Effective Virtual Care
By focusing on robust EHR capabilities and diligent documentation practices, healthcare practices can transform telehealth from a separate task into an integrated, efficient, and effective mode of care delivery. This shift not only streamlines operations for providers and staff but ultimately enhances the accessibility and quality of care for patients, making virtual health a truly integral part of your practice.